A Greater Cost
High-flow nasal cannula (HFNC) treatment for patients with mild to moderate bronchiolitis may be associated with longer hospital stays and higher cost of care, according to a study led by Le Bonheur Hospitalist Jeffrey C. Winer, MD, MA, MSHS, and published in the American Academy of Pediatrics (AAP) journal Hospital Pediatrics. Le Bonheur co-authors included Chief of Pediatric Infectious Diseases Sandra Arnold, MD, Hospitalist Kristen Bettin, MD, MEd, and Chief of Pediatric Hospital Medicine Elisha McCoy, MD.
“Historically, the relationship between HFNC usage outside of the intensive care unit and outcomes including hospital length of stay and cost is unclear. Our study sought to see if HFNC itself may be partially responsible for these outcomes,” said Winer.
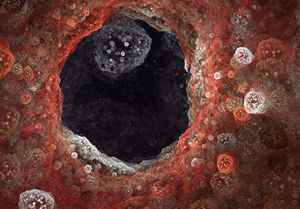
HFNC is a treatment that delivers oxygen to a patient at a high rate, reducing the work of breathing. It is widely used for treating bronchiolitis, a lower respiratory tract infection and a leading cause of emergency room visits for children younger than 2
years. Recent studies on HFNC have shown variable results across patient populations, particularly regarding outcomes such as hospital length of stay (LOS) and cost of care. While severe cases of bronchiolitis where HFNC was used were associated with symptom improvement and decreased LOS and cost, HFNC use in mild to moderate cases has been associated with less symptom improvement, along with increased LOS and cost.
The purpose of this study was to explore the relationship between HFNC usage for non-intensive care unit (ICU) patients and patient outcomes, LOS and cost of care. Researchers reviewed data from 20 hospitals in the Pediatric Health Information System. The data included patients younger than 2 years with a principal or secondary diagnosis of acute bronchiolitis. Researchers categorized these hospitals based on the proportion of non-ICU patients treated with HFNC into low, moderate or high non-ICU HFNC usage (NIHU).

Results showed that LOS was longer for patients in moderate to high NIHU hospitals compared to low NIHU hospitals. Analysis of cost of care showed similar results, where moderate and high NIHU hospitals showed higher costs compared to low NIHU hospitals, even after adjusting for clinical and demographic characteristics. Based on their analyses, researchers estimate that high NIHU hospitals have 5% to 30% longer LOS and 2% to 31% higher cost of care than low NIHU hospitals.
“The large number of patients admitted to children’s hospitals means that even small relative changes in these values may lead to large burdens to hospitals and the health care system,” said Winer.
This study suggests that higher NIHU may lead to increased overall resource utilization for pediatric bronchiolitis patients. More research is needed to assess how HFNC usage affects LOS and cost of care across pediatric hospitals and if HFNC should be limited in non-ICU patients.
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now