Mental Health Epidemic
When Le Bonheur Children’s Hospital opened in 1952, its founders and physicians made a promise to provide the best medical care to all children. In 2023, that promise has taken on a new meaning.
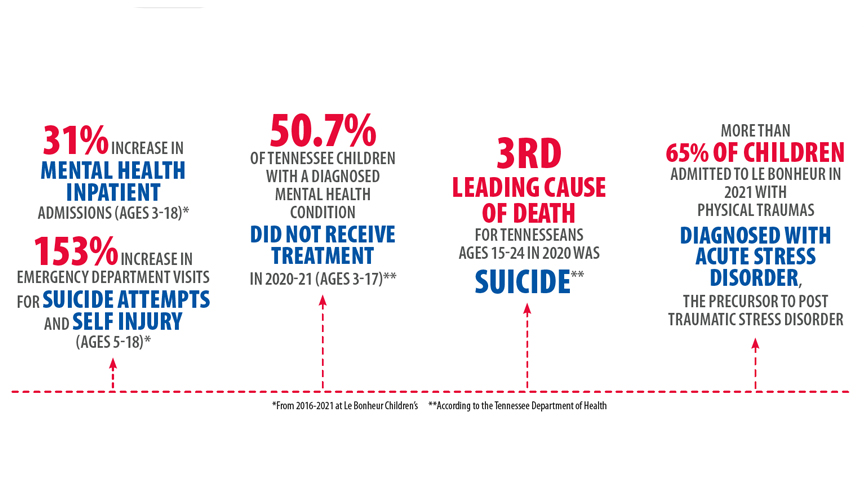
Le Bonheur providers have seen drastic changes in the mental health of kids with sharp rises in mental health inpatient admissions and Emergency Department visits for suicide attempts and self-injury.
“We have to address what the data is telling us on a local, state and even national level,” said Regan Williams, MD, medical director of Trauma Services. “Numbers show that our youth are suffering, and they need our help.”
In the wake of a national mental health crisis largely prompted by the COVID-19 pandemic, providing the best possible medical care to children means providing mental health care, too.
Le Bonheur has responded to this growing concern by establishing multiple mental health programs to care for youth in the Memphis region and beyond. With the goal of addressing mental health inside the hospital and clinic walls, Le Bonheur embedded trained mental health professionals into existing programs to provide immediate care to patients in need, allowing them to begin their recovery process as soon as possible.
The Frontlines of Pediatric Care
In recent years, the hospital’s pediatric primary care group, Le Bonheur Pediatrics, has seen a dramatic increase in patients with mental and behavioral health needs. Lauren McCann, director of Operations at Le Bonheur Pediatrics, sought to address this growing need.
“Pediatricians are the frontlines of pediatric primary care, and they didn’t have the resources to handle the influx of children in need of mental and behavioral health care,” said McCann. “Our pediatricians had to refer patients out to trained professionals, but that meant sending children away knowing that it could be months before they got the care they need.”

Colby Butzon, PhD, (above) is one of six behavioral health consultants integrated in Le Bonheur Pediatrics clinics – Le Bonheur’s pediatric primary care group. Butzon and her team provide behavioral health services, guidance and assistance within the clinics.
McCann knew the answer was to embed behavioral health care into the pediatrician’s office, but the main question was how to do it. After receiving a grant from the Cigna Foundation, McCann built a program with the guidance of Laura Shultz, PsyD, Methodist Le Bonheur Healthcare’s senior director of Ambulatory Behavioral Health, to integrate mental and behavioral health professionals within Le Bonheur’s pediatric primary care practices.
The program, Le Bonheur Pediatrics Behavioral Health, provides behavioral health services, guidance and assistance to patients and families in need. Each of the six Le Bonheur Pediatrics Clinics now has a behavioral health consultant — a trained psychologist, counselor or clinical social worker — who works alongside the pediatrician as part of the patient’s medical team. All behavioral health consultants are supervised by Colby Butzon, PhD.
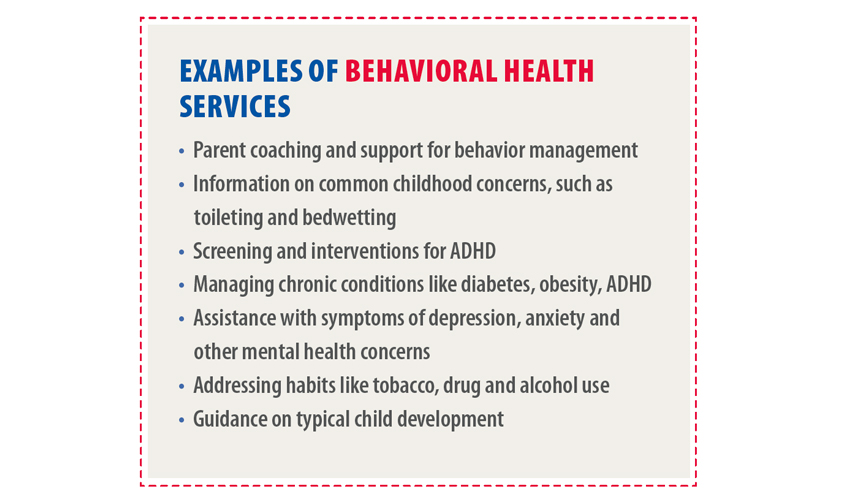
Pediatricians refer their patients to a consultant for a range of concerns, including screening for ADHD and other conditions, behavior problems, school concerns, grief, trauma, depression and anxiety.
“We see patients very quickly, often on the same day,” said Butzon. “Families have been so grateful and even surprised that they are able to get answers to their questions and steps to take to improve their lives so quickly.”
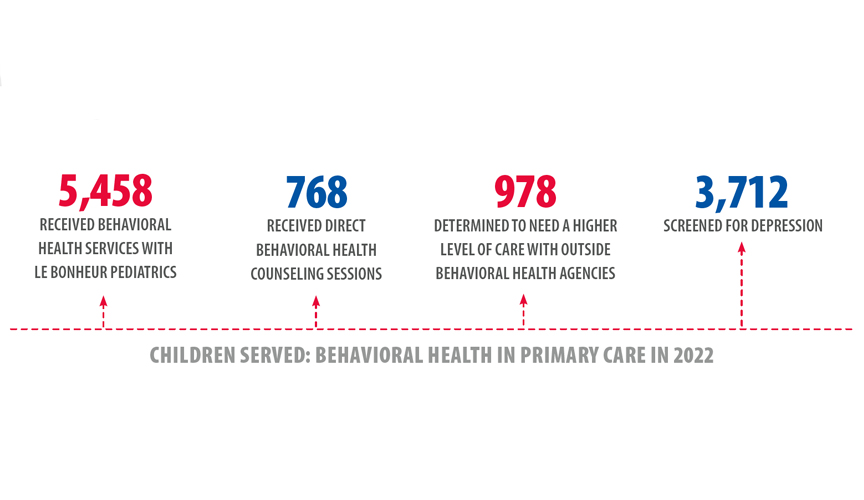
Since 2022, Le Bonheur Pediatrics Behavioral Health has provided services to thousands of children in the community, including depression screenings to more than 3,000 children.
The Behavioral Health program recently created a dashboard to track screening scores and progress for children seen by a consultant. Using this data, the program seeks to disseminate outcome information and demonstrate the program’s effectiveness in providing mental health care to children in the primary care setting.
“Memphis has a particular need for access to behavioral health providers because we have fewer providers per citizen compared to the rest of Tennessee,” Butzon said. “Our goals are to grow the services we provide, support patients across our city and raise awareness of the need for integrated care.”
When Trauma Strikes
According to the Tennessee Department of Health, firearm deaths were the leading external cause of death among Tennessee children in 2021. In response to this uptick in violence and traumatic injuries, Le Bonheur created two programs to provide mental health support for children who experience physical trauma.
Thanks to a partnership with the BRAIN (Building Resilience across Ages through Integrative Neuroscience) Center at the University of Memphis, Le Bonheur began integrating mental health services into the Emergency Department and Trauma division in 2021. Through the program and under the supervision of the BRAIN Center’s Clinical Director of Trauma Services at Le Bonheur Children’s Kiersten Hawes, PhD, LPC-MHSP, ACS, advanced graduate-level students in the Clinical Mental Health Counseling program at the University of Memphis provide free and unlimited counseling services to any child treated at Le Bonheur’s Pediatric Trauma Center. Le Bonheur’s Trauma Center is led by Medical Director Regan Williams, MD, and Trauma Program Director Anissa Cooper, MSN, RN.
“Through our partnership, we’ve already published a study showing that 64.8% of children at our center tested positive for acute stress disorder following a traumatic injury, which is a precursor to post-traumatic stress disorder,” said Williams. “We have a critical need for mental health screening and counseling services at the time of an acute trauma to stop or at least minimize the negative long-term impact on these kids.”

Regan Williams, MD, medical director of Trauma Services at Le Bonheur, has worked to bring multiple programs to Le Bonheur to provide mental health services to children who have suffered a traumatic injury.
Providers meet with children and their families as soon as possible after the trauma occurs. If not seen in the Emergency Department, mental health providers will round with the Trauma team inside the hospital to speak with any child who might benefit from their services.
But there is a particular subset of children who may require more than mental health care alone to avoid the long-term impacts of trauma — children who are victims of violence. In response, Le Bonheur developed the program Supporting and Healing Individuals From Trauma, Hospital-Based Violence Intervention Program (SHIFT-HVIP), a part of the city of Memphis’ violence intervention efforts. SHIFT supports patients and families impacted by violence and provides a wide range of resources, including mental health counseling, school and court advocacy and relocation to safe housing.
“SHIFT provides wraparound services not just to the injured child, but to the entire family,” said Lydia Walker, LMSW, SHIFT program manager. “Every child is part of an ecosystem of a broader family, community and social factors that impact their health, so we want to address as many of these layers as we can.”
When a child comes to Le Bonheur’s Emergency Department with a physical violent trauma, the SHIFT team meets with the patients and family to offer services tailored to their needs. If the family accepts services, mental health counseling is prioritized.
“Our goal is to help children recover both physically and emotionally,” said Williams. “By prioritizing mental health counseling, we are equipping children and families with the tools they need to thrive when they leave the hospital.”

Lydia Walker (right), SHIFT program manager, rounds with the Trauma team to provide wraparound services to families impacted by violence. Through the program, Walker and her team aim to help children recover physically and emotionally.
After connecting the patient and family with a mental health counselor, SHIFT program staff assess the need for other wraparound services. SHIFT has provided families with transportation, coordinated homebound services and education when patients must remain at home post-injury for an extended time and collaborated with schools to re-enroll children who have been out of school for long periods of time.
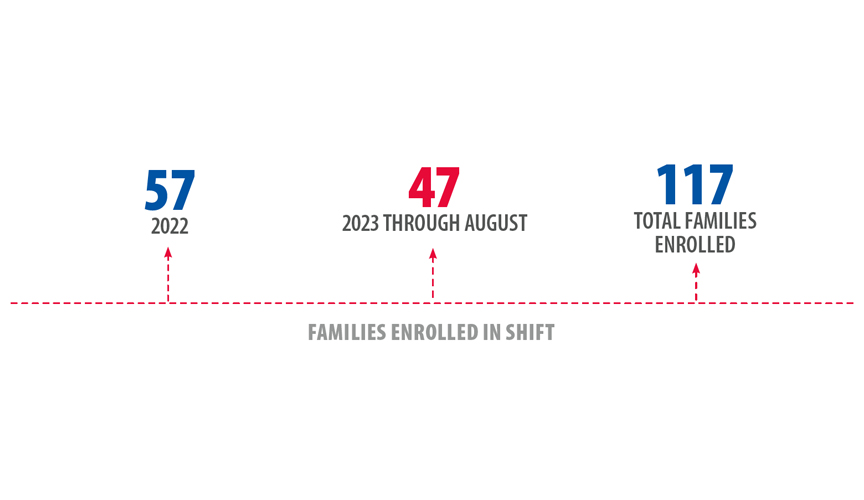
SHIFT works with families for six months to one year. If the family needs more assistance after that, SHIFT connects them to community resource partners like the University of Tennessee Health Science Center and the 901 BLOC Squad, a violence reduction effort in Memphis. Since 2022, more than 100 families have been enrolled in the program.
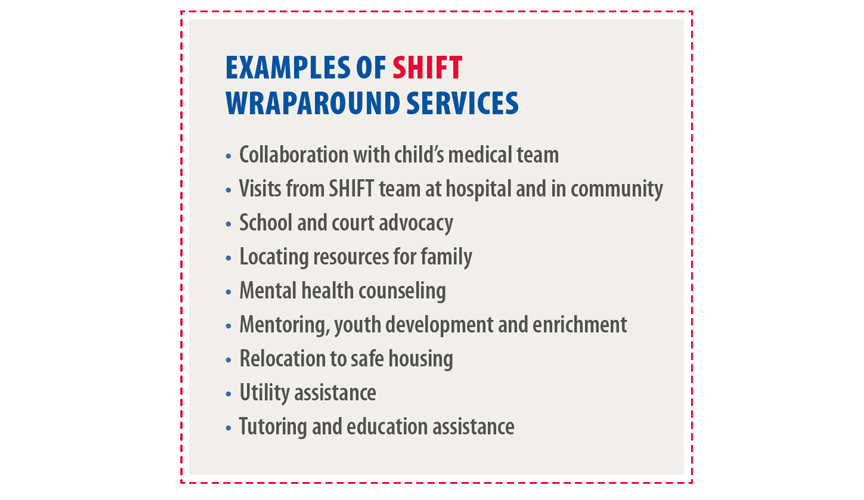
As SHIFT continues to connect families with counselors, mentors and services, Walker hopes to expand program staff by adding more community mentors and create more positive community programs for children to engage in, such as summer camps or job training.
“We need the children in our community to see that there is positivity and opportunity for growth beyond the world they live in right now,” said Walker. “We are all born with dreams, but it’s the possibility of attaining them that makes a difference, so it’s our charge to show them how to map out a way to get there.”
Hope for the Hopeless
As senior director of Emergency Services, Barbie Stewart, RN, MSN, CNL, NE-BC, has experienced firsthand the effects of the mental health crisis currently plaguing youths. The recent influx of children needing psychiatric services into Le Bonheur’s Emergency Department highlighted a significant need for embedding mental health resources into the frontlines of the hospital.
“Patients were coming to us in mental health crisis, and sometimes all we could do was keep them in their room until they could be transferred somewhere else,” said Stewart. “We were inhibiting their road to recovery, and Emergency Department staff members felt that we could do more to help these patients.”
In 2022, Le Bonheur received the “Preventing Youth Suicide: A Cardinal Health Foundation National Collaborative” grant from the Children’s Hospital Association, Cardinal Health Foundation and Zero Suicide Institute at the Education Development Center. Through this grant Le Bonheur created Hope Journey, a program to identify and care for patients in crisis and at risk of suicide. As Hope Journey Committee Chair, Stewart emphasizes the importance of early and active intervention in at-risk patients rather than waiting until a suicide attempt has been made or self-harm has occurred.

Le Bonheur’s Hope Journey leadership team (from left) is Chief Nursing Officer Hella Ewing, RN, MSM, Vice President and Chief Operating Officer Brandon Edgerson, MS, PharmD, Senior Director of Emergency Services Barbie Stewart, RN, MSN, CNL, NE-BC, and Social Worker Nakicia Smith, LCSW. Together they are working to embed mental health resources for children who present at Le Bonheur’s Emergency Department in order to prevent youth suicide.
“You often hear that people contemplating suicide are selfish, but really they have lost all hope and they cannot see a day in the future that would be any better,” said Stewart. “With Hope Journey, we want to give patients a glimpse that things can be better and provide them with the hope they need to keep going.”
A new program at Le Bonheur, Hope Journey is being piloted in the Emergency Department and inpatient units. Patients ages 11 and older admitted to the Emergency Department or directly to the hospital will be screened for suicidal thoughts and depression. A medical social worker will round on patients to guide care based on screening outcomes and connect patients to outpatient counseling or inpatient psychiatric counseling as needed.
Stewart says the goal is to increase comfort level in physicians and staff to help guide patient mental health recovery plans and streamline the process of connecting families to resources through community partnerships.
Goals of Hope Journey also include creating a behavioral emergency response team comprised of trained physicians, social workers, nurses and child life specialists to assist with acute patient events and ultimately avoid restraining, secluding or sedating patients.
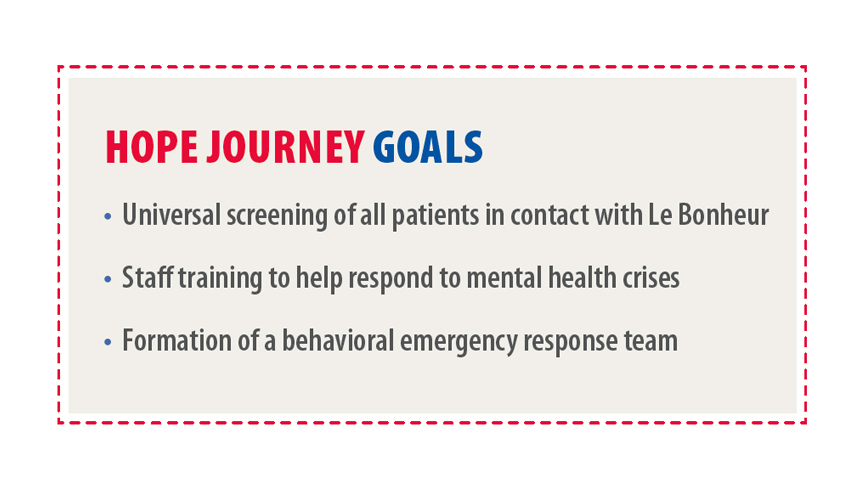
Stewart aims to expand Hope Journey and its screening protocol to all areas of the hospital and clinics to provide the most interventions possible.
“I want our Hope Journey to be all-encompassing,” said Stewart. “We provide hope in so many ways at Le Bonheur, and this program fits in perfectly with the work we already do.”
For Stewart, Hope Journey, along with Le Bonheur’s other mental health efforts, serve as spokes on the wheel of caring for children in the Memphis region. With these programs, Le Bonheur strives to care for the child as a whole, mind and body, and delivers on the promise it made to the community more than 70 years ago.
“We are choosing to tackle this problem because excellent care is part of who we are at Le Bonheur. We promise to care for all children, but if we don’t address the mental health of our patients, then we are not caring for the whole child,” Stewart said.
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now