New device gives epilepsy patient hope
After 10 years of seizures, 23-year-old Hannah Lawrence says she feels hopeful that she may finally be able to move forward with her life.
In January, Hannah, a Le Bonheur Children’s Hospital patient, became the first U.S. patient to receive the NeuroPace® RNS® system at a pediatric hospital outside of the clinical trial. RNS is the first closed-loop responsive brain stimulation system approved by the U.S. Food and Drug Administration for reducing seizures in individuals 18 years of age and older with partial onset seizures.
Ten years ago, Hannah developed what seemed like the flu. But after the flu test was negative and then a seizure left her on the floor, her parents thought something else might be going on. The local emergency room in Brandon, Miss., sent her to Blair E. Batson Children’s Hospital in Jackson, Miss. where she was diagnosed with viral encephalitis. Inflammation of the brain left scar tissue on both sides of her brain, which caused the uncontrolled seizures.
“We didn’t know 10 years ago what we were in for,” said dad, Kenny. “Being new to epilepsy, we thought, well, you go to the doctor and get some medicine and everything will be ok,” said mom Rhonda.
Now the Lawrence family knows that just isn’t the case. Hannah came to Le Bonheur’s Neuroscience Institute in 2007 after her pediatric neurologist in Mississippi encouraged the family to travel to Memphis. James Wheless, MD, co-director of the Neuroscience Institute, and his team have explored every option for Hannah.
“When I first saw Hannah, I knew controlling her seizures would be a challenge. She had already tried several good medical therapies without success. We evaluated her for all other treatment options available and began a plan of therapy. At a comprehensive epilepsy center like the one at Le Bonheur Children’s Hospital, we are able to offer patients like Hannah every option available in the U.S., as we work to control her seizures,” said Wheless.
Before January, Hannah took three different medications – 13 pills – each day. Surgeons implanted a Vagus Nerve Stimulator (VNS) in 2007, and it provided partial relief from her seizures. Hannah had a right temporal lobectomy in 2010 and further brain surgery in 2013. After each surgery, the seizures were reduced, but it wasn’t enough for a teenager to have a normal life.
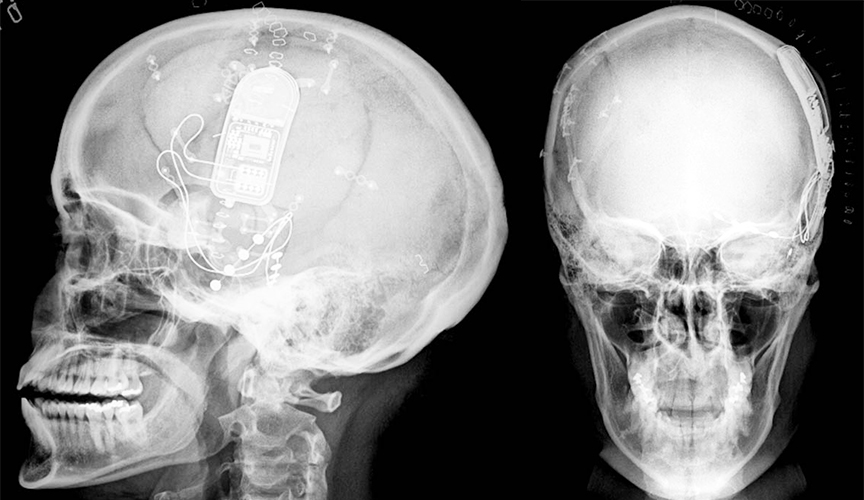
Lateral and AP radiographs of the skull show NeuroPace device overlying the left parietal bone with electrodes extending intracranially.
“Life was pretty tough. She’d have seizures at school. Seizures at restaurants. She couldn’t take a bath alone. She couldn’t lock a door. She has not been able to drive,” Rhonda said.
Day-to-day life was hard – especially during high school. Her mom, Rhonda, eventually quit working because someone needed to pick Hannah up from school after she had a seizure. Hannah missed so much school that she fell behind. Her dreams of going to college were dashed. After high school, she decided to go to barber school to get her barber license and then join her dad in the family barber shop. The Lawrences wanted to give their teenager independence, but when they did, she’d have another seizure. One time she fell and broke her wrist while with a friend.
The family heard about NeuroPace® and started reading online. They called hospitals around the country to see if Hannah could enroll in a clinical trial, but all were full. Once the RNS® was approved by the FDA for those 18 and older, Wheless asked Hannah’s family if they’d consider the device. The Lawrences didn’t hesitate – yes, they wanted the RNS for Hannah. On Thursday, Jan. 22, Le Bonheur Neurosurgeon Paul Klimo, MD, implanted the RNS Neurostimulator within Hannah’s skull and beneath the scalp. The neurostimulator is connected to two leads placed directly on the area of the brain where the seizures are starting from.
“The partnership between the epilepsy team and the neurosurgery team at Le Bonheur has allowed our team to find innovative solutions for patients like Hannah,” said Paul Klimo, MD, chief of Pediatric Neurosurgery for Le Bonheur and Semmes-Murphey neurosurgeon.

Nightly, Hannah pulls out a laptop and a remote monitor to “download her head,” she says. The EEG (brain wave data) information is uploaded to NeuroPace® Patient Data Management System (PDMS), an interactive webbased database used for storage and clinician remote access. Wheless can review the EEG and any seizure activity to adjust Hannah’s medication or the impulses the RNS provides.
Just 48 hours after surgery, Hannah returned home. She returned to work the next Friday. She has been seizure free since surgery.
Hannah and her parents hope the RNS gives her freedom to move forward with life. Hannah has dreams of going to college to become a special education teacher. She wants to drive and be independent.
“I wanted to go to Mississippi State, but that didn’t happen. In high school, I wished I could be a teacher. Now, I’d like to be a special education teacher, because I think I can relate to those kids,” Hannah said.
Two more patients are expected to receive the RNS device this spring.
About NeuroPace® RNS®
- A novel, implantable therapeutic device that delivers responsive neurostimulation and continuously monitors brain electrical activity, detects abnormal electrical activity and responds by delivering imperceptible levels of electrical stimulation to normalize that activity before an individual experiences seizures
- Approved by the U.S. Food and Drug Administration as an adjunctive therapy in reducing the frequency of seizures in patients 18 years of age or older with partial onset seizures who have undergone diagnostic testing that localized no more than two epileptogenic foci, are refractory to two or more antiepileptic medications, and currently have frequent and disabling seizures (motor partial seizures, complex partial seizures and/or secondarily generalized seizures)
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now










