Pinpoint Precision
For Le Bonheur neurosurgeons, to perform a successful epilepsy surgery, they need two critical pieces of information: where a child’s seizures are located and what areas of the brain to avoid to preserve function.
Enter the ROSA One Brain – a robot that provides neurosurgeons with presurgical mapping and precision instrument guidance. ROSA consists of advanced software for mapping and guidance and a robotic arm that the software directs to precise, premapped locations. ROSA fits inside of Le Bonheur’s neurosurgery Operating Rooms (ORs).
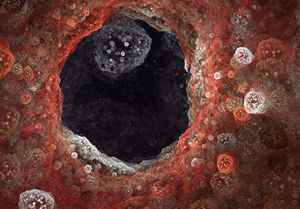
Currently, this technology is used for stereoelectroencephalography (SEEG), a minimally invasive procedure that places a large number of electrodes deep in the brain using incisions of around 2 to 3 millimeters to insert an electrode of just 1.2 mm in diameter. No longer do neurosurgeons have to expose a patient’s brain to place electrodes, and ROSA’s guidance and planning abilities leads to less OR time and higher accuracy.
“When I conduct an epilepsy surgery, my goal is to find the problem and fix it,” said Le Bonheur Neurosurgeon Nir Shimony, MD. “With the ROSA’s capabilities, the chances of finding and fixing the seizure problem areas are much higher and much safer.”
Combining ROSA with Le Bonheur’s full suite of brain imaging products, which includes magnetoencephalography, functional MRI and transcranial magnetic stimulation, Le Bonheur neurosurgeons can create detailed surgery plans to remove seizure areas while also focusing on preserving language, sensory and motor function.

A Precise Operation
Because of ROSA’s precise mapping and guidance, Le Bonheur neurosurgeons can reach previously inaccessible areas of the brain with electrodes in a fraction of the time and with less recovery for the patient. The result of these benefits is a better chance for neurosurgeons to identify seizure locations and create a tailored treatment plan for each child.
From a practical standpoint, SEEG with ROSA is a far easier and safer procedure for children. With its minimally invasive nature, patients can recover more quickly. Conducting a major surgery that removed the skull and exposed the brain, as was needed previously, had an increased potential to lead to bleeding, infection or other surgery complications.
“In a way, SEEG with ROSA is a completely different operation,” said Shimony. “The patient wakes up like you haven’t done anything neurosurgically invasive. Previously we had to open and expose the brain to place grid electrodes and then repeat the same exposure a few days later to remove the grids.”
When preparing for an SEEG procedure, ROSA’s assistance begins before reaching the OR. Combining MRI, CT scans and any other brain imaging from the patient, ROSA creates a comprehensive 3D map of the patient’s brain and head. Using these maps and ROSA’s software, neurosurgeons can create a plan for the trajectory of the electrodes so that they reach precise areas of the brain while avoiding critical structures. This advanced planning typically means less time in the OR and less time a child is under anesthesia.

Once in the OR, ROSA scans the patient’s facial features with a laser and matches the scan to the 3D map of the brain and head. ROSA then guides the surgical instruments to precise locations on the skull based on the surgical plan created before surgery. With just a millimeters large incision, Shimony and his team can place the electrode deep into the brain with an error margin of less than 1 mm.
The time saved with ROSA-assisted SEEG means that neurosurgeons can place more electrodes in less time, which equals a better possibility to identify seizure focus areas. The extensive preoperative planning available with ROSA means that electrode placement accuracy is higher, as the robot guides instruments to their precisely planned locations.
“We used to limit ourselves to four to five electrodes because it took so long and meant that patients were under anesthesia for an extended amount of time,” said Shimony. “This is much easier and safer, so we have the ability to put in more electrodes, potentially finding not only where seizures are coming from, but also where they propagate to. This gives us much better options and a higher chance to have a successful solution for the patients and their families.”
An EEG machine in the OR confirms the placement and function of each electrode. Once finished, the patient’s head is wrapped with a bandage, and they are sent to Le Bonheur’s Epilepsy Monitoring Unit (EMU).
And the process of removing the electrodes is easier, too. If not removed during epilepsy resection surgery, neurosurgeons can remove them with light sedation, closing each incision with just one stitch. With previous methods, the brain would be exposed a second time to remove the electrodes.
All of these benefits combine in an effort to reach the ultimate goal of these neurosurgeons – finding the source of seizures and helping to alleviate the epilepsy burden for patients and families, potentially even eliminating seizures completely. ROSA’s technology gives the ability to pinpoint multiple targets and cover much more space in the brain. Instead of looking at just where seizures start, neurosurgeons can potentially find the extensive networks of the brain that are involved in the seizures.
“ROSA allows us to cover a lot of space in the brain with a better chance to find the problem and benefit the patient,” said Shimony. “In the past, we could find the seizure area about 70% of the time. With ROSA and SEEG, we are up to 90%.”

How It Works: SEEG with ROSA One Brain
- 1. Before surgery, neurosurgeons combine the patient’s brain imaging to create a 3D map of the child’s head and brain with ROSA’s software.
- 2. Using this comprehensive imaging, neurosurgeons make a plan for electrode placement that reaches as much brain area as possible while avoiding critical structures for function.
- 3. In the OR, ROSA uses a laser to scan a patient’s facial features and match them to the 3D map.
- 4. Using the presurgical plan, ROSA precisely guides the surgical instruments to predetermined places on the skull where electrodes will be placed.
- 5. Neurosurgeons make a millimeters small incision and place the electrode deep into the brain.
- 6. An EEG machine in the OR confirms the placement and function of each electrode.
- 7. After all electrodes are placed, the patient’s head is wrapped in a bandage, and they are sent to the Epilepsy Monitoring Unit (EMU) to determine begin the process of determining seizure location.
Advantage Over Epilepsy
This new technology fits in seamlessly with the Le Bonheur Neuroscience Institute’s existing suite of brain imaging – one of the most comprehensive for a children’s hospital in the country. Transcranial magnetic stimulation (TMS), magnetoencephalography (MEG) and functional MRI are all non-invasive technologies that can map the brain’s language, sensory and motor centers to assist with epilepsy surgery planning to avoid these areas.
“Very few centers use all ancillary tests like Le Bonheur does,” said Shimony. “We fuse the results of every test together, which allows us to have a very precise plan regarding anatomy and function of the patient when we proceed with epilepsy surgery.”
While Le Bonheur currently uses ROSA for SEEG procedures, the uses for the technology will continue to grow. Le Bonheur neurosurgeons eventually hope to use ROSA for laser operations that would ablate tumors or deep structures for epilepsy, which will benefit from ROSA’s precision and accuracy.
Minimally invasive surgery continues to be the trend, and neurosurgeons continue to look for ways to do extensive surgeries through a small entry point, says Shimony.
“Having ROSA adds a very robust tool to our suite of technologies,” said Shimony. “We can make data-driven decisions when planning a surgery and provide an easier and more effective seizure localization process for our patients.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now