Even More Heart
Each year, hundreds of families from Memphis — and some from across the country — turn to Le Bonheur’s Heart Institute to receive expert care. Recognized as a top program by U.S. News & World Report, and as an elite pediatric cardiac surgical program by the Society of Thoracic Surgeons, the Heart Institute cared for 433 inpatients, completed 11 heart transplants and implanted 11 ventricular assist devices in 2023.
Le Bonheur’s Heart Institute has experienced significant growth in the past five years. To meet the growing need for pediatric cardiac care, Le Bonheur has created a 31-bed dedicated Cardiovascular Unit, adding 10 Cardiovascular Intensive Care Unit beds to the existing 10-bed unit, and creating room for an 11-bed stepdown cardiac unit.
The Heart Institute expansion also includes a new hybrid Magnetic Resonance Imaging (MRI) and cardiac catheterization (cath) lab. This suite allows experts in Le Bonheur’s Heart Institute to access highly efficient quality imaging, allowing them to make better diagnoses more quickly.
Le Bonheur’s interventional cardiac MRI suite is the first in the state of Tennessee and is only the eighth in the country. The Heart Institute expansion enables Le Bonheur medical staff to care for even more kids and continue to be at the forefront of the latest technology as they constantly find new and improved ways to treat patients safely and efficiently.

Winn Fowler
Winn Fowler’s oxygen level was extremely low following birth. Doctors thought he had inhaled meconium during delivery, and he was taken to the Neonatal Intensive Care Unit at his birth hospital.
During her pregnancy, Winn’s mom, Jessy, underwent a high-risk scan with a specialist to ensure her baby did not have the same cardiac condition as her husband, Jeff. The scan was normal and while Jeff’s congenital heart condition — total anomalous pulmonary venous return (TAPVR) — is not genetic, Jeff still shared his TAPVR diagnosis with Winn’s care team.
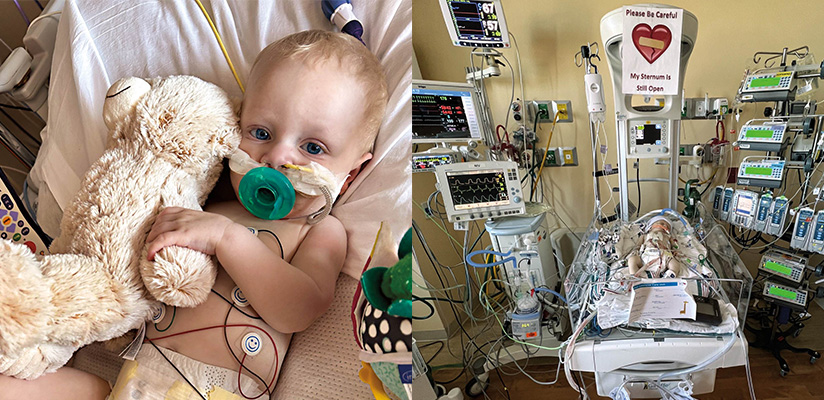
The day after he was born, doctors discovered that Winn also had TAPVR. Winn was immediately transferred via ambulance to Le Bonheur and admitted to the Cardiovascular Intensive Care Unit (CVICU).
At just 2 days old, Winn underwent open heart surgery to reconstruct his veins and get more oxygen to his lungs. His sternum was left open for 24 hours in case doctors needed to operate further. After 10 days in Le Bonheur’s CVICU and seven days in a stepdown unit, Winn was discharged.
In order to prepare his parents for life at home, doctors and nurses provided resources and education on how to administer Winn’s medicine and feed him.
“As new parents, you think of your child as very fragile,” Jessy said. “With a baby who has just had open heart surgery, we especially felt that way. Whatever questions or concerns we had, Winn’s care team at Le Bonheur was there. We never felt alone and always had resources and support in the hospital.”
Winn returned every week for checkups and echocardiograms to make sure his heart was functioning properly. At a routine appointment a few weeks after discharge, the echocardiogram revealed an issue with Winn’s heart.
His care team ordered a heart catheterization in Le Bonheur’s Cath Lab to understand his heart pressure better. Winn’s oxygenated blood was restricted and he had pulmonary stenosis — a condition that causes the heart’s right ventricle to pump harder to get blood to the lungs and can strain the heart.
Winn spent the next eight days in the CVICU and was briefly discharged. At another weekly checkup, doctors determined that 2-month-old Winn would need a second open heart surgery to fix a vein that had been narrowed from scar tissue.
The surgery was a success and for the next six months, Winn received good news at his regular cardiac checkups.
One morning, Jessy went in the nursery to comfort 8-month-old Winn who had woken up crying. She was terrified to discover her son was unconscious. Paramedics were able to stabilize Winn and upon examination, his doctor determined that his heart was failing. Winn needed an emergency heart catheterization and a stent placed immediately.
Following the procedure, Winn’s body did not respond well as fluid built up in his lungs and his heart pressure went back up. Winn’s lungs were shutting down. Jessy and Jeff endured the darkest 24 hours of their lives as doctors worked hard to determine the next best steps for their son.

Winn was diagnosed with a reperfusion injury as his surgically opened veins pumped more oxygenated blood than his body was used to. Fortunately, doctors had a solution, and they were able to alleviate Winn’s condition with steroids.
Winn stabilized and was discharged home on an immune suppression drug to stop his body from scarring the inside of his heart.
Since that stay, Winn had a third successful heart catheterization and doctors hope he will be able to go a full year prior to his next catheterization. Winn returns every month for an echocardiogram to ensure his heart is functioning properly and a check-up with his Le Bonheur cardiologist. Thanks to his care at Le Bonheur, 18-month-old Winn is hitting developmental milestones and thriving.
Hybrid Magnetic Resonance Imaging (MRI)-guided cardiac catheterization (cath) lab opens
Le Bonheur is at the forefront of innovation with the opening of the hybrid Magnetic Resonance Imaging (MRI)-guided cardiac catheterization (cath) lab.
As the discussion of expanding the Heart Institute took place, the radiology and cardiology teams identified the need for a hybrid MRI-cath lab at Le Bonheur as they have conducted many shared cases in the last few years.
According to Le Bonheur Cardiovascular Services director, Crystal Thomas, cath lab cases at Le Bonheur have significantly increased in the past decade growing from 400 per year to more than 650 performed last year. With the addition of more beds in the NICU and CVICU, where 40% of cath lab volume comes from, Thomas expects the number of cath lab procedures to continue to increase.

As case volume grows, the hybrid MRI-cath lab enables more efficient safer patient care.
When using the MRI for imaging instead of a traditional chest X-ray, the patient is not exposed to dye contrast or radiation as the MRI utilizes a magnet. The MRI also provides real-time, functional imaging for providers during cath lab procedures, making the patient’s heart and its anatomic structure easier to visualize leading to improved accuracy.
“This new hybrid MRI-guided cardiac catheterization lab at Le Bonheur is a game changer for us. We will be able to perform heart catheterizations in the MRI environment that will avoid the harmful effects of radiation for our patients,” said Jason Johnson, MD, associate chief of Cardiology and director of Cardiac MRI at Le Bonheur. “Our partnership and collaboration with national technology leaders will provide new diagnostic and interventional procedures for children with heart disease in Memphis and the Mid-South.”
The setup of the hybrid MRI-cath lab suite also leads to patients being under anesthesia for a shorter period as they no longer have to travel between floors for imaging.
“Having the MRI connected to the cath lab creates a safer environment for a patient under anesthesia,” Thomas said. “It also creates a whole new world of opportunities for patient care and procedures in the future.”

There will be a ramping-up period as the radiology and cardiology teams work together to identify cases to utilize the cath lab and MRI at the same time in order to maximize technology to best meet patient needs. The new cath lab and MRI will be used separately most of the time but the hope down the road is to use them in tandem for 30% of cases.
Plans are also in place to transition all cardiac patients to this MRI rather than one on a different floor of the hospital, said Stevie Lee, director of Radiology at Le Bonheur. As Le Bonheur establishes new standards and protocols for the shared space, and with future plans to test new devices and catheters, extensive research will be conducted and eventually published.
Not only will patients benefit from the space, but physicians will be able to showcase their technique and expertise with children’s hospitals around the world. With the capability to live stream from the cath lab, physicians will be able to teach and share
information.
Le Bonheur’s hybrid MRIguided cardiac cath lab continues the Heart Institute’s tradition of excellence and leadership, paving the way for other pediatric cardiology programs. Most importantly, it will allow more kids like Winn and Lawson to receive safe and effective care when they need it most.
Lawson Nichols
“Your baby is missing half of his heart.”
Emily and Martin Nichols were shocked to receive this news the day after their third son, Lawson, was born in a hospital near their Mississippi home. Emily’s pregnancy had been healthy and uneventful with normal routine testing and diagnostics.
Lawson needed immediate critical care from a pediatric heart specialist. Despite being several hours from home, Lawson was flown via helicopter to Le Bonheur where he was admitted to the Cardiovascular Intensive Care Unit.
That same day, a failed congenital heart screening and an echocardiogram revealed Lawson’s condition.
“From the moment we got to Le Bonheur, they took care of us and made us feel reassured,” Emily said. “Lawson was not just another patient and his doctors made us feel heard.”
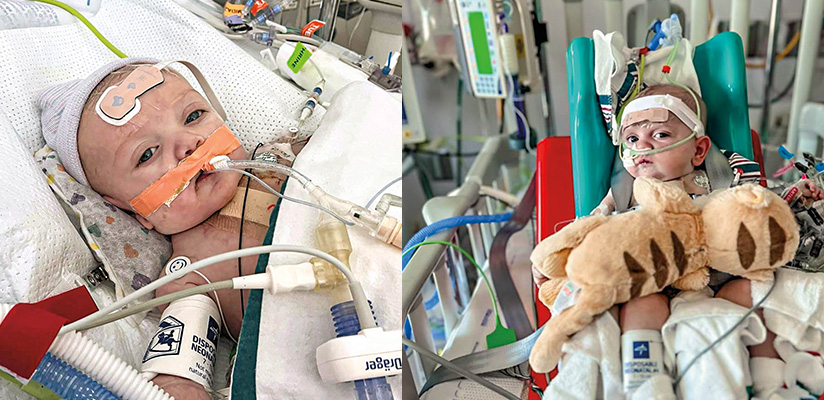
Lawson was diagnosed with four congenital heart defects, including hypoplastic left heart syndrome.
Following rounds of testing and imaging, doctors determined Lawson was stable enough to go home after 10 days in the CVICU.
At a scheduled catheterization procedure a few months later, doctors discovered his heart function had decreased. Lawson needed surgery to reroute his blood flow and improve his heart function. Lawson’s care team prepared his parents for the surgery and explained what to expect. For two days, a ventricular assist device (VAD) helped Lawson’s heart pump blood.
Lawson slowly improved and a week after surgery, he was extubated and weaned off oxygen. Lawson grew stronger as he underwent physical therapy sessions and received nutrition via an NG tube in his nose while he recovered. While doctors initially thought Lawson might need to remain at Le Bonheur until his next surgery, he was able to go home from the CVICU after one month.
Initially, Lawson was on an external pacemaker to regulate his heart rate, but he no longer required it or any other equipment. Lawson is able to control his heart function with several medications and his parents are able to feed him via a bottle.
For now, the Nichols family returns to Le Bonheur every other week so Lawson can be monitored at the high-risk cardiac clinic and undergo an echocardiogram. Emily and Martin check in daily with Lawson’s care team via an app and submit his oxygen levels, which they monitor at home with a pulse oximeter and his weight. These statistics are monitored closely as weight loss or a decline in heart function are indications that another cardiac surgery is needed.

Lawson will receive long-term care at Le Bonheur’s Heart Institute and doctors anticipate he will need another surgery in the next few years. Emily and Martin know when that day comes, their son will be in the best hands.
“We are so grateful for Le Bonheur,” Emily said. “They saved our son’s life and Lawson’s care team feels like family. Whatever challenges present themselves in the future, we know Lawson will receive the very best care at Le Bonheur.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now