Virtual Blueprints
Le Bonheur Interventional Cardiologist Neil Tailor, MD, and Cardiovascular Surgeon Umar Boston, MD, faced an obstacle. A patient had developed a clot in a recently placed bioprosthetic valve and urgently needed another valve replacement. But the patient was in such poor condition that further surgery was not an option. Instead, Boston requested that Tailor perform a cardiac catheterization and place a valve inside of the patient.
This technique is known as a percutaneous mitral valve-in-valve replacement and is not commonly performed in children. But Boston and Tailor had one major advantage for the smoothest and safest possible procedure — virtual reality (VR).
“Positioning and placement of the valve was critical, and we needed to think outside of the box for this case,” said
Boston. “The VR technology provided another option for planning and precise placement of the implant that avoided another open heart surgery.”

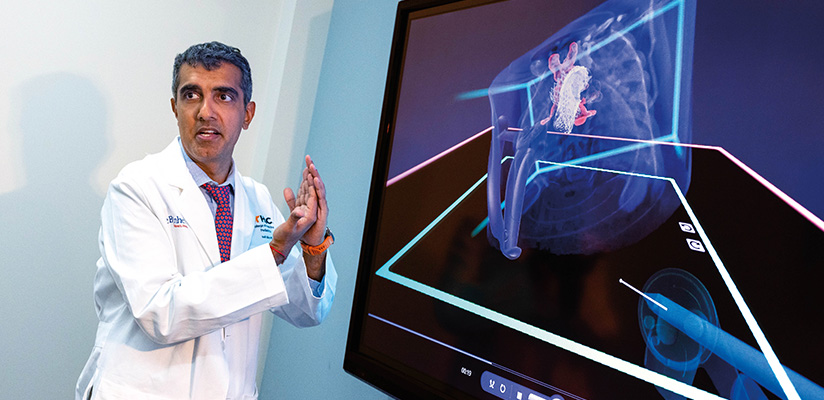
Tailor, who founded the Le Bonheur Heart Institute Virtual Reality Program, created a 3D model of the patient’s heart and the valve to be implanted. Using VR technology, he planned the procedure by placing the 3D model of the valve in the 3D model of the heart in a virtual space to determine the best position for the valve and to see how this placement related to other structures in the heart.
This VR planning led to a straightforward, successful percutaneous valve-in-valve replacement that was completed within 30 minutes.
“Thanks to VR we can grab and hold the simulated heart, place devices and position them where needed,” said Tailor. “VR allows us to get inside the heart defect and create a more precise plan ahead of surgeries and procedures.”
Le Bonheur Children’s Hospital is one of only a few pediatric centers in the world using VR to plan heart surgeries and cath lab procedures. This precise planning leads to safer and faster surgeries and procedures for patients at Le Bonheur’s Heart Institute.
Dynamic Perspectives
When Tailor was searching for his niche in the cardiology field, VR modeling immediately stood out. While the software used was initially created for planning otolaryngology (ENT) and skull surgeries, it also has proved to offer opportunities in treating congenital heart disease.
In 2022, Tailor established the Le Bonheur Heart Institute Virtual Reality Program.
“VR allows us to model procedures in the cath lab and surgical operating room in a more dynamic way. Existing imaging gives, at best, a 3D reconstruction of a heart that is similar to looking at drawings in a book. With VR, we can move around inside the heart as if we are holding it in our hands,” said Tailor.
To build these 3D models, Tailor uses raw data from a patient’s CT scan, MRI or 3D echocardiogram. And to create the most accurate models, Tailor does not rely completely on computer algorithms. He segments the data himself taking the patient’s 2D scan and turning it into a 3D model for the highest level of accuracy. With time, he has also built a library of 3D models of every device that Le Bonheur interventional cardiologists and surgeons might use by scanning them with a fluoroscopy machine.
Tailor and Boston work together to discuss cases and determine which ones might benefit from VR planning. In the cath lab, Tailor uses VR for every patient who already has a CT scan. For surgical cases, Boston finds that VR planning is useful in more providing myriad benefits — for themselves as physicians but also for their patients.
“Previously, we had limits on planning before cath lab procedures. We would look at an ECHO and CT scans, but have to figure out many details of the procedure as we went along,” said Tailor. “With VR, we’re moving away from that and can plan substantially more beforehand.”
The planning capabilities that VR provides before a cath lab procedure means shorter procedure time, as well as less high-radiation imaging and contrast for the patient. Plus, the VR plan provides a reference for correct device placement that cardiologists can use in the cath lab to verify the device’s correct location.
Boston sees similar benefits for his heart surgeries that can be planned with VR. The extensive planning that VR allows means his patients have less time under anesthesia and less time on heart-lung bypass during surgery.
“If you have a well-orchestrated plan, it’s better over time and down the road for patients,” said Boston. “VR gives us another way to fine-tune our management strategy from a preoperative standpoint.”
A New Dimension
A key focus for the expansion of this program is further developing the use of VR for heart transplants — even when determining whether a donor heart will fit a recipient’s chest cavity. While Boston can currently use VR to plan parts of the heart transplant surgery, the hope is that soon he will be able to use a 3D scan of the donor’s heart and a 3D scan of the recipient’s chest cavity to virtually place the donor heart into the recipient’s chest.
This builds upon work already underway in Le Bonheur’s Heart Transplant Program to better match recipients with the proper donor heart. Working with radiologists, Boston and his team have developed a database of chest cavity volumes and associated weights to help surgeons determine the appropriate donor weight range for patients waiting for a heart. VR would take this a step further, providing another checkpoint for accurately matching a donor and recipient.
VR has implications for the education of the next generation of physicians, too, says Tailor. Currently, cardiologists in training learn in 2D, but the ability to view the heart through VR means 3D perspectives as well as the ability to see specific slices of the heart and overlay different areas.
Tailor and Boston feel so strongly about the potential for VR that Le Bonheur is incorporating a VR lab into the recently opened Heart Institute expansion. This expansion adds a hybrid cardiac MRI and cath lab to the two existing cath labs, all on the same floor as the Cardiovascular Intensive Care Unit and CV Operating Room. The VR station will allow families the opportunity to see their child’s heart defect and cath lab procedure plan to better understand exactly what’s going on with their child’s heart.
“For families, it’s helpful to see their child’s heart in 3D, and with the dedicated cardiac MRI, we’ll be able to use that imaging to build our 3D models with no radiation for the patient,” said Tailor. “Eventually we hope to use VR for 4D modeling — allowing us to plan surgeries and procedures on a VR heart that is pumping blood and beating.”
Help us provide the best care for kids.
Le Bonheur Children's Hospital depends on the generosity of friends like you to help us serve 250,000 children each year, regardless of their family’s ability to pay. Every gift helps us improve the lives of children.
Donate Now